Refeeding Syndrome and its Management
Management of
Refeeding Syndrome
Essential Minerals and Vitamins: A Clinical Guide to Prevention and Treatment
Critical Care
Metabolic Medicine
Key Priorities
Thiamine (B1)
Neurological protection
Phosphorus
Cellular energy
Potassium
Cardiac stability
Magnesium
Enzyme function
Critical: Thiamine must be administered before or concurrently with nutritional support to prevent Wernicke’s encephalopathy.
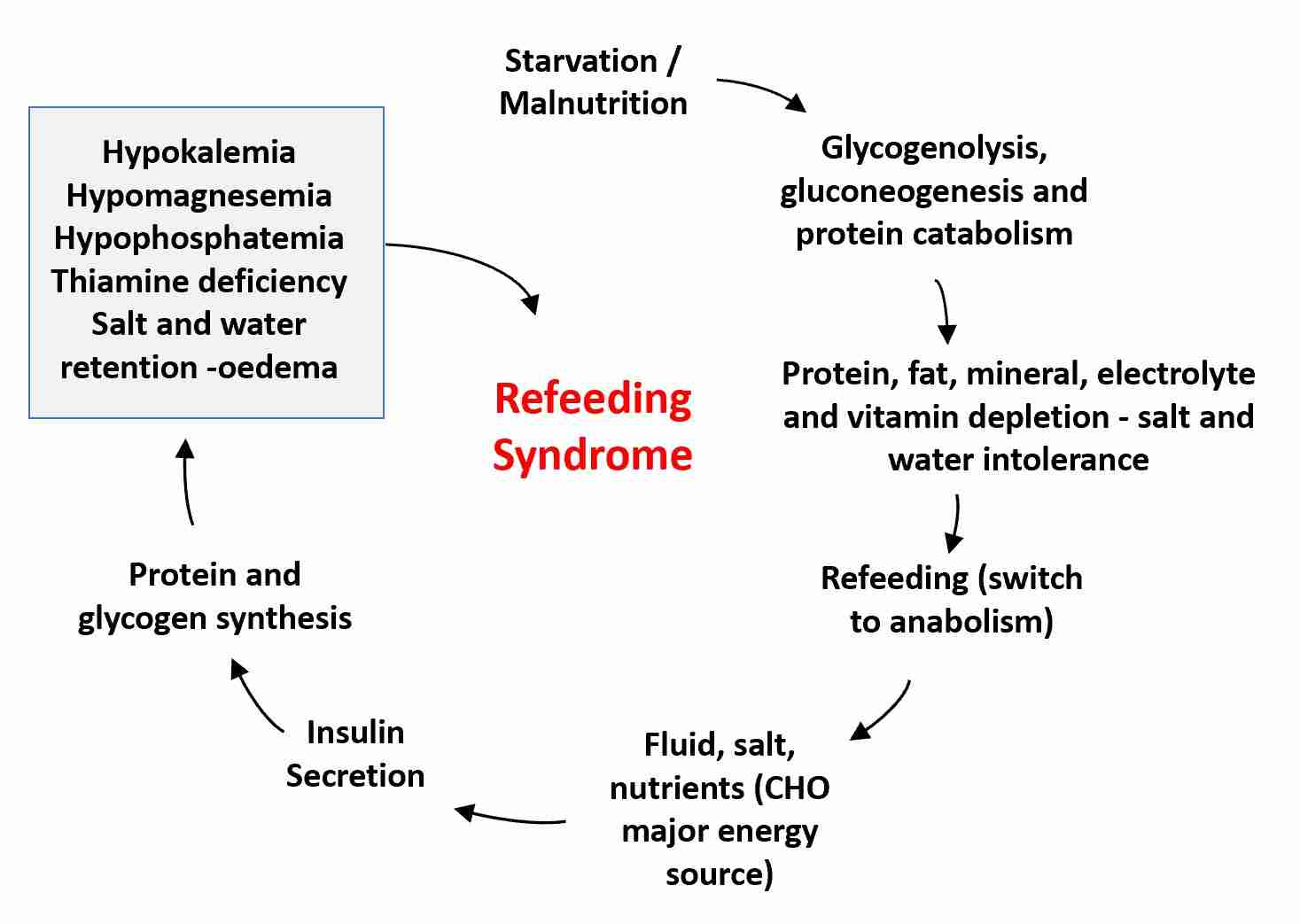
Understanding Refeeding Syndrome
Definition and Pathophysiology
Refeeding syndrome (RFS) is a potentially life-threatening condition characterized by severe electrolyte and fluid shifts that occur when nutrition is reintroduced to a malnourished or starved individual
[1],
[2].
Metabolic Transition
During prolonged fasting, the body adapts by shifting from carbohydrates to fat and protein stores for energy. This state is marked by decreased insulin and increased glucagon, leading to gluconeogenesis, lipolysis, and ketogenesis [2].
When refeeding begins, particularly with carbohydrates, there is a rapid increase in insulin secretion. This promotes cellular uptake of glucose, phosphate, magnesium, and potassium, causing a precipitous drop in their serum concentrations
[1], [2].
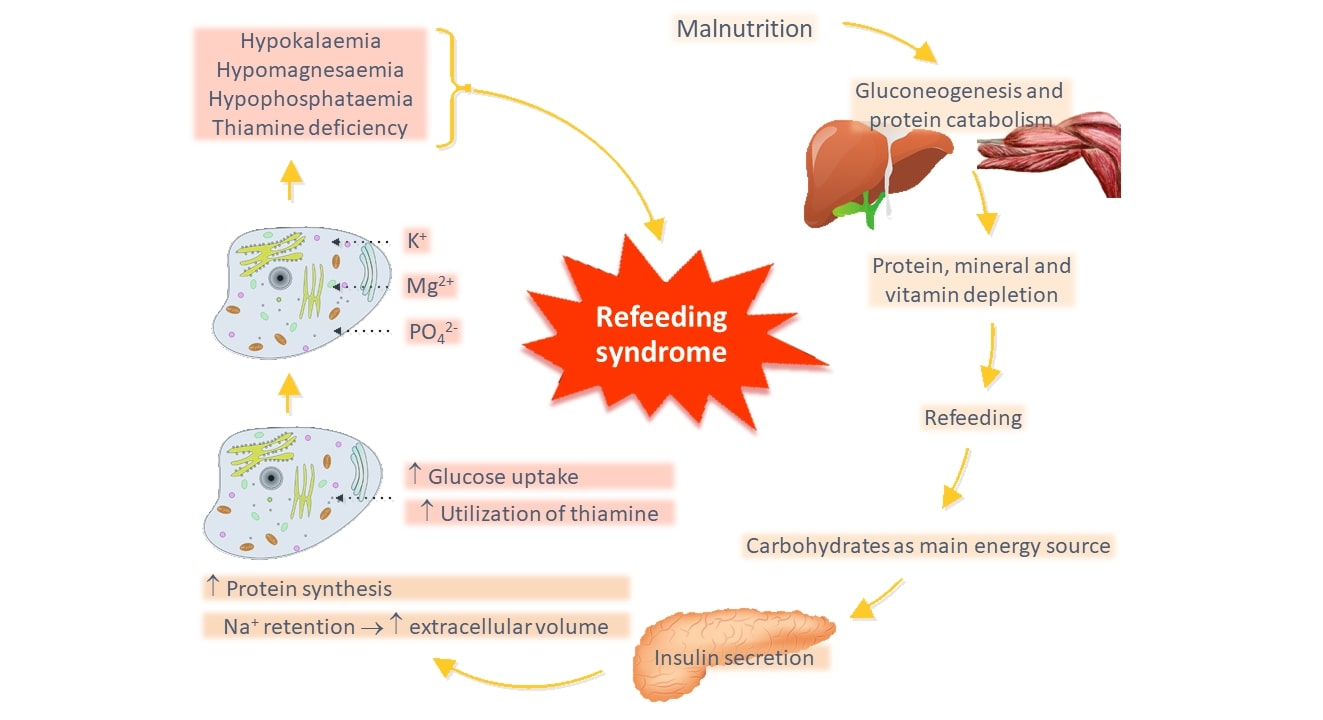
Starvation Phase
Basal metabolic rate decreases by 20-25%. Intracellular mineral stores become depleted while serum levels may appear normal.
Refeeding Phase
Insulin surge drives electrolytes into cells, exacerbating pre-existing deficits and causing clinical manifestations.
Risk Factors and Patient Identification
High Risk Criteria (NICE)
Patients are considered high risk with one or more of:
BMI < 16 kg/m²
>15% unintentional weight loss (3-6 months)
Little or no nutritional intake for >10 days
Low pre-feeding K+, PO₄³⁻, or Mg²⁺ levels
Source: NICE Guidelines
Additional Risk Factors
Anorexia nervosa (especially BMI <14 kg/m²)< /span>
Chronic alcoholism
Cancer, malabsorption syndromes
Prolonged fasting (postoperative, hunger strikers)
Drugs: Insulin, chemotherapy, diuretics, antacids
Important: Serum electrolyte levels may be normal prior to feeding due to homeostatic mechanisms. This should not be interpreted as low risk of RFS. Clinical assessment is crucial [1].
Key Electrolyte Imbalances
Hypophosphatemia
Most prominent electrolyte disturbance
Impairs ATP production, oxygen delivery, cell membrane integrity
Hypokalemia
Major intracellular cation
Vital for nerve conduction, muscle function, cardiac stability
Hypomagnesemia
Cofactor for 300+ enzyme systems
Essential for ATP production, neuromuscular function
Core Minerals and Vitamins in RFS Treatment
Thiamine (Vitamin B1)
Thiamine is prioritized first to prevent Wernicke’s encephalopathy, a rapidly progressing neurological emergency
[1],
[2].
Critical Roles:
Cofactor for pyruvate dehydrogenase complex (glycolysis to Krebs cycle)
Essential for transketolase in pentose phosphate pathway
Prevents lactic acidosis from impaired glucose metabolism
Wernicke’s Encephalopathy Triad:
- Ophthalmoplegia (eye movement abnormalities)
- Ataxia (unsteady gait)
- Confusion
Can progress to Korsakoff’s syndrome if untreated [5].
Phosphorus (Phosphate)
Phosphorus is fundamental to cellular energy metabolism through ATP and regulates oxygen delivery via 2,3-DPG
[2].
Clinical Consequences of Deficiency:
Cardiac: Impaired contractility, arrhythmias, heart failure
Respiratory: Muscle weakness, respiratory failure
Neurological: Confusion, seizures, coma
Hematological: Hemolysis, leukocyte dysfunction
Supplementation Protocol
Oral Maintenance
0.3-0.6 mmol/kg/day
[2]
IV Correction
9 mmol over 12 hours [2]
18 mmol over 12 hours [2]
Caution: Risk of hypocalcemia and metastatic calcification with rapid IV infusion, especially in renal impairment.
Potassium
Potassium is the principal intracellular cation, vital for membrane excitability, nerve conduction, and muscle contraction
[2].
Critical Functions:
Maintains cardiac rhythm and prevents arrhythmias
Essential for skeletal and respiratory muscle function
Regulates cell volume and intracellular pH
Hypokalemia Complications:
- • Cardiac arrhythmias (ventricular tachycardia/fibrillation)
- • Muscle weakness, paralysis
- • Respiratory muscle failure
- • ECG changes: flattened T waves, U waves
Replacement Guidelines
General Requirement
2-4 mmol/kg/day in RFS [1]
IV Correction (NHS)
Important: Correct hypomagnesemia simultaneously as magnesium deficiency exacerbates hypokalemia [1].
Magnesium
Magnesium serves as a critical cofactor for over 300 enzymatic reactions and is essential for electrolyte balance
[2].
Essential Roles:
ATP production (glycolysis, Krebs cycle)
DNA/RNA and protein synthesis
Cardiac rhythm maintenance
Potassium and calcium homeostasis
Replacement Strategy
Maintenance
IV Correction (NHS)
Cardiac monitoring recommended during IV infusion due to risk of bradycardia and hypotension.
Importance and Roles of Key Nutrients
Metabolic Pathways
Phosphorus: ATP Synthesis
Essential for energy storage and transfer through ATP. During refeeding, increased metabolic activity demands substantial ATP, leading to rapid cellular phosphate uptake [2].
Potassium: Membrane Potential
Maintains resting membrane potential crucial for nerve impulse transmission and muscle contraction. Insulin promotes Na+/K+-ATPase activity during refeeding [2].
Enzyme Systems
Magnesium: Cofactor Function
Required for over 300 enzymatic reactions including ATPases, glycolytic pathway, and Krebs cycle enzymes. Crucial for DNA/RNA synthesis and protein production [2].
Integrated Metabolic Picture
A[“Refeeding
Carbohydrate Intake”] –> B[“Insulin Surge”]
B –> C[“Cellular Uptake”]
C –> D[“Electrolyte Shifts”]D –> E[“Hypophosphatemia”]
D –> F[“Hypokalemia”]
D –> G[“Hypomagnesemia”]
E –> H[“ATP Depletion”]
F –> I[“Cardiac Arrhythmias”]
G –> J[“Enzyme Dysfunction”]
H –> K[“Cellular Dysfunction”]
I –> K
J –> K
L[“Thiamine Deficiency”] –> M[“Wernicke’s Encephalopathy”]
L –> N[“Lactic Acidosis”]
style A fill:#9CAF88,stroke:#374151,stroke-width:2px,color:#fff
style M fill:#DC2626,stroke:#374151,stroke-width:2px,color:#fff
style K fill:#EA580C,stroke:#374151,stroke-width:2px,color:#fff
style L fill:#F59E0B,stroke:#374151,stroke-width:2px,color:#fff
Prioritization of Nutrient Supplementation
Thiamine
Neurological emergency prevention
Electrolytes
Phosphate, Potassium, Magnesium
Multivitamins
Comprehensive support
Thiamine: The Critical First Step
Thiamine supplementation is universally prioritized as the initial and most critical step due to the rapid and severe neurological consequences of deficiency, particularly Wernicke’s encephalopathy [1], [2].
Rationale for Priority:
Onset can be rapid (within days)
Can cause permanent neurological damage
Medical emergency requiring immediate treatment
Administration Protocol
Before or concurrently with nutritional support
Especially if carbohydrates are part of refeeding regimen
Electrolytes: Addressing Immediate Shifts
Following thiamine, the next priority is prevention and correction of electrolyte disturbances: hypophosphatemia, hypokalemia, and hypomagnesemia
[1], [2].
Hypophosphatemia
- • Rhabdomyolysis
- • Respiratory failure
- • Cardiac dysfunction
- • Seizures
Hypokalemia
- • Cardiac arrhythmias
- • Muscle weakness
- • Paralysis
- • ECG changes
Hypomagnesemia
- • Cardiac arrhythmias
- • Neuromuscular irritability
- • Worsens hypokalemia
- • Enzyme dysfunction
Guidelines for Supplementation and Monitoring
Pre-Feeding Assessment
Essential Laboratory Tests
Electrolytes: Phosphate, Potassium, Magnesium, Sodium, Calcium
Glucose and renal function
Nutritional markers: Zinc, B12, Folate, Iron studies
Cardiovascular assessment
Clinical Evaluation
Anthropometrics: BMI, recent weight loss
Nutritional history: Duration of poor intake
Medication review: Diuretics, antacids, chemotherapy
Alcohol and substance use
Recommended Dosages and Administration
| Nutrient | Dosage | Route | Key Considerations |
|---|---|---|---|
| Thiamine (B1) | Oral: 100 mg t.d.s.
IV: Pabrinex 1 pair b.d. (5 days) Pediatric: 1-2 mg/kg/day |
Oral, IV over 30 mins | Highest priority. IV for high-risk patients. Monitor for reactions. |
| Phosphate | Maintenance: 0.3-0.6 mmol/kg/day
IV Moderate: 9 mmol/12h IV Severe: 18 mmol/12h |
Oral, IV (dedicated line) | Risk of hypocalcemia, metastatic calcification. Monitor levels. |
| Potassium | Requirement: 2-4 mmol/kg/day
<3.0: 40-80 mmol/day 3.0-3.5: 20-40 mmol/day >3.5: 10-20 mmol/day |
Oral, IV (KCl) | Monitor K+ and renal function. Correct hypomagnesemia. |
| Magnesium | IV: 0.2 mmol/kg/day
Oral: 0.4 mmol/kg/day <0.5: 20-40 mmol/day 0.5-0.75: 10-20 mmol/day |
IV (slow), Oral | Cardiac monitoring during IV. Essential for K+ correction. |
| Multivitamins | Once daily for 7-10 days
Pediatric: 5 days or until 100% RDI |
Oral, Enteral, IV (PN) | Addresses broader micronutrient deficiencies. |
Monitoring Protocols During Refeeding
Clinical Monitoring
Vital Signs
Every 4-6 hours initially for high-risk patients. Bradycardia can be early sign of RFS
[4].
Cardiac Monitoring
Continuous ECG for very high risk patients or cardiac conditions [1].
Neurological Status
Level of consciousness, confusion, seizures, ataxia.
Fluid Balance
Strict intake and output monitoring daily [3].
Critical Time Frame
The first 72 hours after initiating feeding are particularly crucial, as this is when RFS is most likely to develop [1].
Other Nutritional Considerations
Multivitamin and Trace Element Supplementation
In addition to critical nutrients, guidelines recommend administration of balanced multivitamin and trace element preparations to address broader micronutrient deficiencies [1], [3].
Components Typically Included:
Vitamins
- • B complex (B2, B6, B12)
- • Folate
- • Vitamin C
- • Vitamin D, E, K
Trace Elements
- • Zinc
- • Selenium
- • Copper
- • Chromium
Administration Guidelines
Duration: First 7-10 days of refeeding
Examples: Forceval, Sanatogen A to Z, or IV preparations for PN patients [1].
Caloric Intake and Progression
The fundamental principle is to “start low and go slow”
[5]. This approach minimizes metabolic stress and electrolyte shifts.
Initial Caloric Targets
5-10 kcal/kg/day
10-20 kcal/kg/day
50% of requirements
Progression Guidelines
- • Increase gradually over 4-7 days
- • Monitor biochemical and clinical status
- • Involve dietitian in planning
- • Balance carbohydrate load (aim for ~40% initially)
Complications of Untreated RFS
Cardiac Complications
Neurological Complications
Critical Prevention Message
These complications are largely preventable through proper risk assessment, thiamine prophylaxis, electrolyte monitoring, and gradual refeeding. Early recognition and prompt treatment are essential to prevent permanent damage or death.
References
https://www.uhbw.nhs.uk/assets/1/23-639_refeedingsyndromeguideline-4_redacted.pdf
https://pmc.ncbi.nlm.nih.gov/articles/PMC2440847/
https://myconnect.swbh.nhs.uk/wp-content/uploads/2024/02/Refeeding-guidelines.pdf
https://www.rch.org.au/uploadedFiles/Main/Content/gastro/Refeeding%20syndrome%20guideline.pdf
https://www.sciencedirect.com/topics/psychology/refeeding-syndrome


